Breadcrumbs
Emergency Intubation
Emergency Intubation for Impending Respiratory Failure
- Medical personnel must wear aerosol generating procedure PPE before any airway management procedure. Observe airborne, droplet and contact transmission precautions.
- Must don PPE properly and optimally for full protection with supervision. Do not rush.
- Minimize the number of personnel in the room during resuscitation.
- Compared to Protected Code Blue, there may be more time to optimize patient’s oxygenation prior to intubation depending on the situation.
- Hypnotic drugs and muscle paralysis are needed in a conscious patient with respiratory failure prior to intubation.
- Encourage early intubation to prevent additional risks to staff performing emergency intubation to manage severe hypoxia, and to avoid prolonged use of high flow nasal oxygen or non-invasive ventilation.
- This is a physiological difficult airway:
- Anticipate rapid oxygen desaturation to a critically low level after induction and muscle paralysis as these patients have minimal reserve.
- Also, anticipate hypotension - consider administering a prophylactic dose of vasopressors/inotropes +/- IV fluids bolus BEFORE induction drugs. Prepare for hemodynamic instability during and after airway management.
- Reccomend generous gel application to lubricate the endotracheal tube to facilitate smooth passage into the larynx because the patient's oral cavity and upper airway may often be extremly dry.
PREPARATION
Environment
- Preferably resuscitation is performed in an isolation room with negative pressure ventilation; if not possible, ensure all doors are all closed.
- Minimize the number of door opening and people entry during resuscitation
Equipment
- Prefer using disposable equipment over reusable equipment whenever possible.
- Use a dedicated COVID emergency airway resuscitation cart carrying a cardiac monitor, intubation equipment and drug supply and other essential supplies. Most protocols recommend discarding all unused disposable items in the room after resuscitation thus bring in only essential items into the room. (show a dedicated cart and content)
- Drape to cover resuscitation cart, monitors and other airway equipment.
Equipment & drugs INSIDE the Room
Airway, oxygen and ventilation equipment
- A dedicated emergency airway resuscitation cart with cardiovascular and oximetry monitors.
- Confirm room oxygen supply, nipple, suction before entry into room
- Ventilation & oxygenation equipment
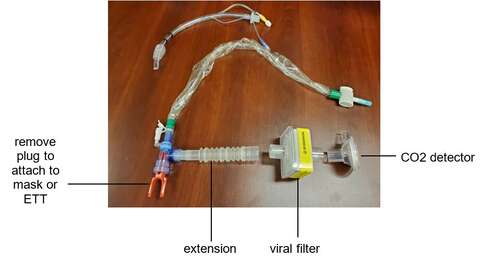
- Ambu / Laerdal bag & mask
- inline suction system
- airway extension (tube catheter mount)
- breathing HEPA viral filter
- CO2 detector (assemble equipment before entering the patient’s room)
- Airway and intubation equipment:
- video laryngoscope + blades (e.g, C Mac with #3 and D blades)
- oral airways
- ETT tubes (consider evac ETT for prolonged ICU intubation)
- malleable stylet
- syringe to inflate cuff
- ETT securing device / tape
- Yankauer suction
- tracheal tube introducer (bougie)

- Anesthetic drugs:
- propofol / ketamine / midazolam
- rocuronium / succinylcholine
- fentanyl as needed
- phenylephrine
- Consider preparing an emergency intubation box containing a disposable stethoscope, role sticker, pen, plastic cover for paper record, checklist for transportation and other essential items.
Drugs and Equipment OUTSIDE the Room
Airway, oxygen and ventilation equipment:
- second generation LMA (size 3, 4, and 5)
- gel pack to lubricate ETT / LMA if necessary (dry secretion)
- difficult intubation cart including fiberoptic intubation and surgical airway kit.
Other equipment - cardiac arrest cart
PATIENT & MEDICAL TEAM
Patient
- Most likely these patients are in respiratory distress with some degree of hypoxemia and are receiving high O2 concentration via a non rebreathing mask, high flow nasal oxygen or non invasive ventilation. Note that it is recommended to avoid NIV due to its unproven utility in ARDS and the risk of virus aerosolization.
- Leave oxygen device on until intubation to minimize droplet and airborne spread.
- Suggested criteria of endotracheal intubation: no improvement in respiratory distress, tachypnea (respiratory rate greater than 30 / min), and poor oxygenation (Pao2 to Fio2 ratio < 150 mmHg) after 2-h high-flow oxygen therapy or noninvasive ventilation
Reference - Chinese Society of Anesthesiology Task Force on Airway Management Chinese Society of Anesthesiology Task Force on Airway Management, Expert recommendations for tracheal intubation in critically ill patients with noval coronavirus disease 2019 Chin Med Sci J 2020 DOI: 10.24920/003724)
Medical Team
- Conduct an expedited review of pertinent patient history, cardio-respiratory status, oxygenation status, COVID status, and appropriateness of resuscitation outside the room. Confirm DNR status.
- Clearly delineate roles, use closed loop communication and articulate clear plan for resuscitation and airway management.
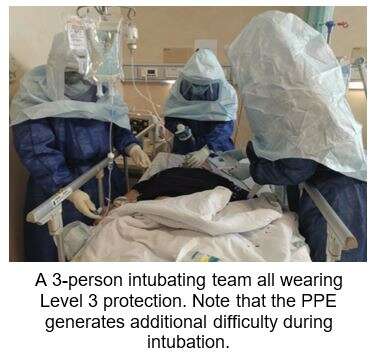
- Hospital protocol varies regarding the number of medical personnel in the resuscitation room. The overall goal is to limit the number of people in the room.
- At a minimum, the team inside the room will consist of:
- experienced airway operator - anesthesiologist or ER or ICU doctor
- airway assistant - respiratory therapist (RT)
- registered nurse (RN) to assist with monitor and drug administration; Outside the room: 1-2 door runners - RN and unit attendant to respond to equipment / drug needs.
- All resuscitation team members don FULL personal protective equipment (PPE) properly before entering the room. Do not rush. (see PPE section)
- Assign a clean safety officer (spotter) to supervise donning and doffing PPE.
- Leave all non essential personal items outside the room.
- Full PPE consists of:
- a disposable Association for the Advancement of Medical Instrumentation (AAMI) level III fluid resistant long sleeve gown;
- long cuffed gloves (double)
- eye protection (goggles)
- full face shield
- fit tested N95 respirator
- neck bib protector
- hair cover / hood.
Follow local hospital infection prevention and control protocol.
- Some protocols recommended Level 3 PPE protection and this is conducted as follows: hand disinfection → head cap → protective mask N95 → surgical masks → isolation gown → disposable latex gloves → goggles → protective clothing → disposable latex gloves → shoe covers → disposable gown → disposable latex gloves → full head hood (Mengqiang Luo MQ et al. Precautions for Intubating Patients with COVID-19. Anesthesiology, 2020).
- VIDEO
Humber River Hospital Protected Code Blue Strategy
- The reason for a second layer of disposable gown and glove is the option of removing the outer layer once intubation is completed. This will minimize the risk of contamination to any equipment or furniture in resuscitation room.
- Wash hand with disinfectant-containing alcohol whenever possible after a contaminated task.
- Record names of all participating staff members in case of contact tracing.
- Simulation training is strongly recommended for preparation ahead of emergency intubation surge.
AIRWAY MANAGEMENT
Pre-oxygenation
- Outside the resuscitation room, set up the Ambu / Laerdal bag & mask in the following sequence: face mask, inline suction, airway extension, filter, extension, CO2 detector, ventilation bag, and oxygen supply tube (see picture). Tighten all connections.
- Use a high efficiency hydrophobic heat and moisture exchanging (HME) filter with 99.99% bacterial/viral efficiency.

- Once entered room, place drugs and airway equipment on a table, and position video laryngoscope stand in appropriate locations around the bed.
- Check oxygen supply and suction system.
- Assess patient’s level of consciousness, vital signs and respiratory effort.
- Most likely the patient is on high flow oxygen. Turn off oxygen flow before removing patient’s procedural mask and oxygen mask to minimize viral aerosolization.
- Apply resuscitation face mask and use a 2 hand vice grip technique to maintain a good mask seal.

- Avoid assisted bag mask positive pressure ventilation if at all possible.
- If assisted bag mask positive ventilation is absolutely necessary, recommend covering the area around the patient’s mouth and nose with a wet gauze to help prevent virus spreading (reference Precautions for Intubating Patients with COVID-19).
- Meticulous pre-oxygenation with 100% oxygen with a well-fitting mask for 3 - 5 min if possible depending on patient’s baseline oxygen saturation level and acuteness of the situation. Monitor to check if patient’s oxygen saturation rises with pre-oxygenation.
- Suggest use low oxygen fresh gas flow (e.g., 5 liters/min) if possible. Watch the reservoir bag filling and collapsing to judge adequacy of ventilation.
- Do not use HFNO using nasal prong for pre-oxygenation or apneic oxygenation because of the risk of aerosolization.
- Our local experience suggests that patients who are tachypneic and hypoxic while wearing a non rebreathing mask on 100% oxygen are unlikely to respond to another 3-5 min of face mask pre-oxygenation. Suggest proceed directly to intubation.
Intubation

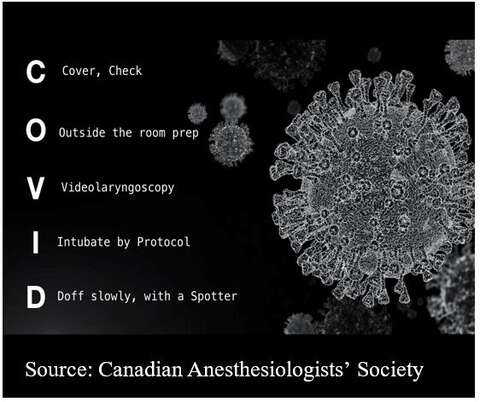
| 
| 
| 
|
- Lubricate the endotracheal tube liberally with get to facilitate intubation because patient airway is anticipated to be extremely dry.
- Anticipate rapid oxygen desaturation after induction and muscle paralysis in COVID patients who have preexisting pulmonary dysfunction.
- Perform rapid sequence induction (RSI) and intubation.
- Anticipate severe hypotension after anesthetic induction if the pateitne has baseline hypovolemia. Prepare for vasopressor support and volume resuscitation.
- In an awake patient, suggest use propofol, midazolam or ketamine as appropriate for induction.
- Profound muscle paralysis before instrumenting the airway to avoid coughing.
- Suggest use rocuronium >1.5 mg/kg and wait for 15 to 20 sec before intubation.
- Recommend the most experienced anesthesiologist to intubate assisted by an experienced RT / AA.
- Prefer to use video laryngoscopy as a first line approach to visualize and confirm airway intubation. Recommend using disposable blades e.g., C-MAC and McGrath laryngoscope or a single use disposable video laryngoscope.
- Pay attention to the intubation posture. Suggest the airway operator to stand upright and step back to maximize the distance between the airway operator’s face and the patient during intubation.
- Place video laryngoscope and all airway equipment into a dirty bin in one move; seal for decontamination.
- Once intubation is completed, inflate endotracheal tube (ETT) cuff fully and reconnect ETT to Ambu / Laerdal bag and filter immediately. Check for cuff leak before starting positive pressure ventilation.
- Confirm positive CO2 detection.
- Avoid manual IPPV using face mask before intubation; if necessary for rescue oxygenation, use minimal tidal volume and low ventilation pressure using 2 person vice grip technique with an oral airway.
- After successful intubation, suggest remove outside contaminated gloves if double gloving and remove contaminated gown if no PPE shortage.
- Confirming the depth of the ETT is difficult using auscultation while wearing PPE. Suggest point of care ultrasound to confirm bilateral lung movement and a CXR later to confirm ETT tip location.
- Fogging of eye goggles and poor visibility can be a serious problem during RSI intubation. A possible solution is to apply a layer of anti-fogging agent, such as transparent hand sanitizer to the inside of the goggles.
- May insert a nasogastric tube (per local resuscitation protocol) to minimize the need for another close contact with the airway.
Manual Ventilation
- Ventilate per clinical requirement.
- Anticipate a slow rebound in oxygen saturation. Apply PEEP for manual bag ventilation as appropiate.
- Large volume ventilation and recruitment maneuvers to correct hypoxemia immediatelly after tracheal intubation should be avoided (reference: Yao W et al. Emergency tracheal intubation in 202 patients with COVID-19 in Wuhan, China: lessons learnt and international expert recommendations. Br J Anaesth 2020)
- Avoid any unnecessary circuit disconnection.
- When the circuit disconnection is necessary e.g., changing from manual to mechanical ventilation, stop manual ventilation, clamp ETT (e.g., with Kelly forceps); always leave the HME filter attached to the ETT before disconnection to prevent viral aerosolization.
- Always make a clear loud announcement to alert team members in the room when disconnect ETT from resuscitation bag.
Failed Intubation
If failed intubation despite video laryngoscopy and bougie intubation, suggest:
- Insert oral airway.
- Reapply mask using a 2 hand vice grip technique to maintain a good mask seal.
- Use minimal tidal volume and low ventilation pressure for manual ventilation.
- Alternatively, insert immediately a supraglottic airway device e.g., Intubating LMA or air-Q to further decrease air leak and as a conduit to facilitate intubation.
- Note the reliability of seal is greatest with tracheal tube > supraglottic airway > face mask.
- If condition permits, consider doing an asleep fiberoptic intubation under video laryngoscopy.
- Last resort for a can’t intubate can’t oxygenate (CICO) situation, use emergency front of neck access (eFONA) technique.
Anticipated Difficult Airway

| 
|
- Prepare plans A, B and C and discuss among airway team members.
- Recommend 2 anesthesiologists to manage the airway.
- After induction and muscle paralysis, perform video laryngoscopy with a styleted ETT as the first choice since this is a familiar technique to most anesthesiologists. If unsuccessful, attempt using a tracheal tube introducer (bougie) immediately.
- If video laryngoscopy with bougie is unsuccessful, proceed to fiberoptic intubation alone or combined with video laryngoscopy.
- Limit the number of fibertopic intubation attempts while monitoring for signs of severe oxygen desaturation.
- If absolutely necessary to assist ventilation as rescue, apply 2 hand vice grip gentle face mask ventilation with minimal tidal volume and peak pressure to maintain oxygenation.
- Quickly switch to a supraglottic airway device e.g., Intubating LMA or air-Q to further decrease air leak and as a conduit to facilitate intubation.
- Avoid awake fiberoptic intubation at all cost.
- Proceed to an emergency front of neck airway (eFONA) if can’t intubate and can’t oxygenate. The scalpel-bougie-tube technique is particularly preferred in COVID-19 patients over the cannula techniques because it does not require oxygen insufflation thus minimize the risk of aerosolisation.
AIRWAY: INTUBATION TEAM CONCEPT
Key Points
- Emergency intubation in a COVID-19 patient with respiratory failure and hypoxia is one of the highest risk maneuvers because it carries a heightened risk of viral spread to healthcare workers.
- Instead of letting any physician to manage the airway in such a dire situation, the intubation team concept was introduced in Wuhan, China to limit the risk of infection to healthcare workers.
- This airway / intubation team comprises a group of experienced airway experts, mostly anesthesiologists, to provide a dedicated intubation service that may be required several times per hour.
- Members of this team must be well trained and follow strict protocols to limit viral exposure.
- Because these airway / intubation team members are more frequently exposed to COVID-19 infection risk, some centres recommend a Level 3 PPE protection - hand disinfection → head cap → protective mask N95 → surgical masks → isolation gown → disposable latex gloves → goggles → protective clothing → disposable latex gloves → shoe covers → disposable gown → disposable latex gloves → full head hood (Mengqiang Luo MQ et al. Precautions for Intubating Patients with COVID-19. Anesthesiology, 2020).
- Below are some examples of airway / intubation team protocol, checklist, documentation and team member roles and responsibilities.
Trillium Health Partners
Toronto Western Hospital
TRANSFER TO ICU
- Ideally there will be 2 teams, team 1 (the resuscitation team) to prepare the patient for transport and team 2 will receive the patient outside the room to minimize the risk of contamination. Both teams will wear PPE per hospital policy.
- If there is only 1 team, the resuscitation team members must change to clean PPE before transfer.
- Always clamp the ETT when switching from one method of ventilation to another and remove the clamp when ready to ventilate again.
- Always keep HME filter connected to ETT whenever disconnect circuit.
- Maintain muscle paralysis to avoid coughing during transfer.
- Maintain sedation where appropriate with small aliquots of propofol, midazolam or ketamine.
- Remove contaminated gown and gloves and change to clean PPE before leaving the resuscitation room.
- Assign a dedicated person who will NOT contact the patient to open doors and operate elevators etc. Other transport team members do not touch any doors or other hospital equipment during transport.
- On arrival to the ICU, repeat same disconnection procedure (stop ventilation, clamp ETT, disconnect from Ambu / Laerdal bag and connect to ICU ventilator; declamp ETT and start ventilation. Always leave the filter connected to the ETT.
- Do not leave any contaminated items on patient’s bed.
INFECTION CONTROL & DEBRIEF
- Document intubation procedure.
- Remove PPE per local hospital protocol before leaving the resuscitation room and ICU. Doffing is preferably done in an anteroom if available. If not available, remove gloves and gown in the resuscitation room and remove face shield and mask outside the room.
- Doffing with utmost care; use buddy system and use a checklist.
Donning doffing PCB - VIDEO
- Wash hands after each step of doffing.
- Remember to remove the N95 mask last when doffing.
- Some protocols suggest changing scrub and taking a shower after having been involved in a COVID case.
- All surfaces of non disposable equipment and supply must be wiped down after resuscitation per hospital policy.
- Discard all contaminated disposable equipment per hospital protocol.
- Team debriefing
- Staff to complete personal log book of clinical exposures
ADDITIONAL RESOURCES
Recommendations for Endotracheal Intubation of COVID-19 Patients
Tracheal intubation in patients with COVID-19
Click HERE for additional resources.
