Breadcrumbs
Anesthesia in Patients with Positive COVID Status or Suspected Positive
PERIOPERATIVE MANAGEMENT STRATEGY
| 
|
Key Points
- Preferably perform only emergency surgery (limb or life threatening) to preserve hospital capacity and minimize risk to healthcare providers and patients.
Infection Control
- protect self and other medical personnels e.g., full PPE for airborne precautions, limit staff in the OR
- protect environment and equipment e.g., use a dedicated COVID room and equipment, do surgery in a negative pressure ventilation room if available
- prevent airborne transmission, e.g., personnel wearing PPE including N95 masks, recognize aerosol generating events e.g., high risk during intubation and especially during extubation (coughing) and high risk surgeries e.g., airway surgery.
- prevent droplet transmission, e.g., patient wearing a surgical mask and oxygen mask before induction
- prevent contact transmission, e.g., double gloving and fluid resistant gown to prevent self contamination
- apply aerosol minimizing strategies e.g., apply HME filter to breathing circuit, avoid bag mask ventilation when the airway is not isolated.
Choice of anesthesia
| 
|
- If general anesthesia is indicated, endotracheal intubation is recommended for COVID positive / suspected patients to reduce risk of patients coughing and risk of droplet and aerosol transmission.
- Spinal anesthesia is recommended for cesarean delivery in a mother with COVID-19 but the mother must wear a surgical or N-95 mask. Note that thrombocytopenia may occur in patients with advanced or systemic COVID-19 thus exclude regional anesthesia.
- Peripheral nerve block can be performed with proper precautions e..g, full PPE for medical providers and place a clear drape over the patient’s face. This is particularly important during upper limb block when the clinician is doing the procedure close to the patient’s face and mouth. Suggest use a non rebreathing filter mask (e.g., Tavish mask) or if not available, apply both a procedural mask and a oxygen mask over the patient’s face during case. Sedate lightly and cautiously especially in patient with preexisting respiratory compromise.
PREOPERATIVE PREPARATION
Environment
- Proceed in a dedicated COVID room, preferably with negative pressure ventilation.
- If not available, proceed with doors closed and minimize the frequency of door opening during case. The recommended minimum OR air exchange is 20 air exchanges per hour.
- Signage should be placed outside room to indicate COVID-19 Patient – Air-borne Precautions.
- Designate only one mode of entry into the room, minimize opening and closing of that door
Equipment
- Prefer to use disposable equipment over reusable equipment whenever possible.
- Use a dedicated airway and drug cart containing only essential supplies for the case because all unused items in the room will be disposed afterwards.
- Keep main drug cart, difficult airway cart and cardiac arrest cart outside the room as back up.
- Drape to cover anesthetic machine, monitors and computers for electronic charting.
- It is hard to do paper charting without contamination. Proceed per local hospital policy. Recommend to discard pen at the end of case.
- Keep hand sanitizers in OR for frequent hand clean as often as necessary.
Patient
- Often the patient is on supplemental oxygen through a nasal cannula / oxygen face mask. Place a procedural mask on the patient in addition to the nasal cannula / oxygen mask during transport and leave them on until time of pre-oxygenation to minimize droplet and airborne spread. Note: place the oxygen mask over the procedural mask on the patient.
- Suggest use the lowest possible supplemental oxygen flow through nasal cannula / face mask (e.g., ≤ 5 liters/min) to maintain oxygen saturation and to minimize the risk of viral aerosolization.
- Consider using a filter non rebreathing mask (e.g., Tavish mask with viral/bacteria filters attached to the mask side ports, see picture) if available. (Somogyi R et al. Chest 2004;125:1155-7).

- Transport patient to OR along a designated route with minimal contact with other patients and staff.
- Pertinent preoperative patient history also includes fever, respiratory symptoms, complete blood count, nucleic acid test, and / or serological antibody test.
Medical Team
- All OR personnel (anesthesia and surgical teams) don FULL personal protective equipment (PPE) for airborne precaution and keep full PPE on for the duration of surgery. (see more on PPE section)
- PPE consists of:
- a disposable Association for the Advancement of Medical Instrumentation (AAMI) level III fluid resistant long sleeve gown
- gloves (double)
- eye protection (goggles)
- full face shield
- fit tested N95 respirator
- hair cover / hood.
- Recommend use long cuffed surgical gloves or non-sterile nitrile gloves that are long enough to cover the sleeves of the gown completely to prevent contact transmission.
- Some protocols recommend additional shoe cover and neck cover and in specially high risk infectious situation, use a powered air purifying respirator (PAPR).
- Every effort is made to reduce the risk of self contamination via mucous membranes especially during the time of doffing. This includes potential droplet contamination to the neck, lower pants, shoes and inner gown (contact transmission).
- Best to assign a designated clean safety officer (spotter), usually a nurse, to supervise donning and doffing PPE.
- Minimize the number of personnel in the room during the case.
- Suggested team composition inside the room:
- airway and anesthesia operator - anesthesiologist
- airway assistant - respiratory therapist (RT) / anesthesia assistant (AA)
- in room runner - circulating registered nurse (RN)
- the surgical team.
Outside the room: 1-2 door runners - RN and OR attendant to respond to equipment / drug needs.
- Leave all non essential personal items outside the room. Only assigned safety officer can retrieve additional material from the cart throughout the case.
- Clearly delineate roles, use closed loop communication and articulate clear plan for airway & anesthesia management.
- Communication with portable phone using speaker phone feature. Avoid putting phone next to face and ear.
- Record names of all participating staff members in the OR in case of contact tracing.
- Simulation training is strongly recommended ahead of crisis.
INTRAOPERATIVE PRE-OXYGENATION
- Recommend to use a closed circuit (e.g. anaesthetic circle) or a re-breathing circuit (e.g. Mapleson’s C (‘Waters’) circuit to trap virus-containing exhaled gas.
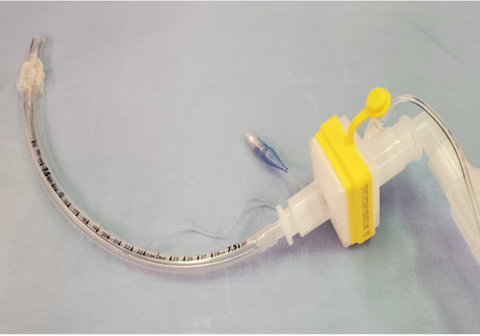
- Use breathing circuits that are fitted with a high efficiency hydrophobic heat and moisture exchanging (HME) filter with 99.99% bacterial/viral efficiency. Suggest connect HME filter directly to face mask (see picture)

- Tighten all anesthetic circuit connections to avoid accidental disconnection which increases the risk of viral aerosolization.
- Minimize the interval between removal of patient’s PPE and application of face mask.
- Recommend 2 trained staff to perform pre-oxygenation and intubation.
- Use a 2 hand vice grip technique to maintain a good mask seal (see picture)

- Check for mask leak - a triangular rather than square ETCO2 trace or a low numerical ETCO2 value during pre-oxygenation suggests a leak around the face mask.
- For additional aerosol minimizing precaution, consider cover the patient’s face with a plastic drape during pre-oxygenation and intubation (see additional information)
- Meticulous pre-oxygenation with 100% oxygen with a well-fitting mask for 3-5 minutes. Aim to achieve ET O2 >85% if possible.
- Suggest use low oxygen fresh gas flow (e.g., 5 liters/min) if possible. Ensure the adjustable pressure-limiting (APL) valve is fully open. Watch the reservoir bag filling and collapsing to judge adequacy of ventilation.
- Avoid HFNO for pre-oxygenation or apneic oxygenation using nasal prong because of risk of aerosolization.
- Recommend to apply a second HME viral filter in the expiratory limb of the circuit to trap virus-containing exhaled gas and reduce the risk of contamination to the anesthetic machine.
- Keep the surgical team outside the OR until intubation is completed.
INTRAOPERATIVE: INTUBATION
| 
|
- Must perform a quick but precise airway assessment preoperatively. Note that detailed airway assessment can be challenging when the patient is wearing a surgical mask and oxygen mask.
- Anticipate rapid oxygen desaturation in COVID patients who have preexisting pulmonary dysfunction and hypoxemia.
- Perform rapid sequence induction (RSI) and intubation.
- Place all induction and intubation drugs and equipment on a stand. Avoid contaminating other equipment and cart in the room.
- Some protocols suggest ketamine 1 mg/kg and lidocaine 1.5 mg/kg for induction.
- Profound muscle paralysis before instrumenting the airway to avoid coughing.
- Suggest use rocuronium >1.5 mg/kg or succinylcholine 1.5 mg/kg; caution: succinylcholine induced hyperkalemia may occur if patient has hypercapnea + respiratory acidosis. Wait for 15-30 sec for full paralysis before intubation attempt.
- Recommend the most experienced anesthesiologist to intubate assisted by an experienced RT / AA.
- Prefer to use video laryngoscopy as a first line approach to visualize and confirm airway intubation. Recommend to use disposable blades e.g., McGrath laryngoscope, or apply a plastic sheath over the CMAC blade.
- Once intubated, inflate endotracheal tube (ETT) cuff and reconnect ETT to filter immediately. Check for cuff leak (may use a cuff manometer) before starting positive pressure ventilation.
- Avoid manual IPPV using face mask before intubation; if necessary, use minimal tidal volume and low ventilation pressure using 2 person vice grip technique with an oral airway.
- Place video laryngoscope and all airway equipment into a dirty bin in one move; seal for decontamination.
- Secure ETT well to avoid the need of ETT misplacement, depth adjustment or re intubation.
- Tighten all circuit connections.
- After successful intubation and ETT securement, remove outside contaminated gloves if double gloving and change to a clean gown if no PPE shortage.
- Some protocols recommend placing a wet gauze on the patient's mouth and nose after intubation to reduce the risk of droplet transmission during positive pressure ventilation.
INTRAOPERATIVE: FAILED INTUBATION
| 
|
Limit to a maximum 3 attempts with video laryngoscopy and bougie intubation.
If failed intubation, suggest
- Insert oral airway.
- Reapply mask using a 2 hand vice grip technique to maintain a good mask seal.
- Use minimal tidal volume and low ventilation pressure for manual ventilation.
- Alternatively, insert immediately a second generation supraglottic airway (e.g., Supreme LMA, i-gel, and ProSeal LMA).
- Use the lowest possible tidal volume and peak pressure for manual ventilation; avoid leak around supraglottic airway.
- Plan to do asleep fiberoptic intubation under video laryngoscopy.
- Last resort for can’t intubate can’t oxygenate (CICO) situation, use emergency front of neck access (eFONA) technique.
- Avoid awake fiberoptic intubation.
INTRAOPERATIVE: MECHANICAL VENTILATION
- Plan ventilation management ahead (e.g., protective lung ventilation strategy, high PEEP etc.).
- Use lowest gas flow to maintain oxygenation.
- Monitor airway pressure. Note that inline filter in the expiratory limb may increase airway pressure and auto PEEP.
- Maintain muscle paralysis.
- Elevate head of bed 45 degrees if appropriate.
- For any circuit disconnection, stop ventilation, clamp ETT (e.g., with Kelly forceps); always leave the HME filter attached to the ETT before disconnection to prevent viral aerosolisation.
- In patients presenting ARDS, consider lung protective ventilation strategy:
- tidal volumes 4-8 mL/kg predicted body weight
- Pplateau < 30 cm H2O
- Permissive hypercapnia, target pH 7.20 – 7.45
- For patients with ARDS, consider PEEP & FiO2 (5 for 0.3, 5-8 for 0.4, 8-10 for 0.5, 10 for 0.6)
- tidal volumes 4-8 mL/kg predicted body weight
- Conservative fluid strategy if appropriate.
INTRAOPERATIVE EXTUBATION
- Be conservative. If there is any doubt about patient’s respiratory status after extubation, keep the patient intubated and ventilated and transfer patient to the ICU.
- The time of anesthesia emergence and extubation demands extra attention and precautions because this is a high risk aerosol generating event.
- The surgical team is recommended to leave the OR at this time. Only the 2 member airway team and a RN remain in the room.
- Again apply aerosol minimizing strategy at the time of extubation e.g., avoid coughing, droplet contamination and viral aerosolization.
- Suction while the patient is still paralyzed and asleep thus no coughing.
- If available, use a closed suction system to minimize viral aerosolization (see picture).

- Use a 2 person extubation technique.
- Strategies to avoid patient coughing - consider deep extubation if appropriate; consider iv lidocaine, remifentanil and dexmedetoxidine as appropriate.
- Some protocol recommends applying a clear drape over face to contain aerosolization in anticipation of post extubation coughing (see picture).

- WATCH VIDEO (extubation at minute 4:00)
- Exercise extreme caution when removing the clear drape as it contains aerosolized particles.
- Remove ETT that is connected to the filter and the anesthesia circuit as a single unit to avoid aerosolization (picture). Do not disconnect ETT from filter.
- Either leave the contaminated ETT underneath the drape or discard it carefully into a dirty garbage bin in one move.
- Then apply a face mask with the HME filter under the drape immediately after extubation

- Switch back to a non rebreathing filter oxygen mask when the patient is settled and is not coughing. Do not use a venturi mask or nasal prong.
POSTOPERATIVE CARE
Routine Recovery
- Recover the patient by the anesthesia team or a PACU nurse (if appropriate) in the OR for ≥ 30 min for air exchanges in a positive ventilation room with the doors closed. Droplet precaution is sufficient after this wait period.
- Wait until the patient is stable and not coughing before heading to the PACU.
- Administer anti-emetics as appropriate to reduce the risk of retching, nausea and vomiting. Do not use dexamethasone for possible risk of steroid in COVID patients.
- Reapply a regular procedural mask and oxygen mask on the patient.
ICU Transfer
- Before transfer, stop mechanical ventilation, clamp the ETT tube (e.g., Kelly forceps) to avoid aerosolization of respiratory secretions; always keep the HME filter connected to the ETT, disconnect the filter from anesthesia circuit and then connect to a Ambu / Laerdal bag or a dedicated COVID-19 transport ventilator. Always clamp the ETT when switching from one method of ventilation to another.
- Relieve clamp to continue ventilation.
- Maintain anesthesia and muscle paralysis to avoid coughing during transfer.
- Remove contaminated gown and gloves and change to clean PPE before leaving the OR.
- Assign a dedicated person to open doors, elevators, etc who will NOT contact the patient. Other transport team members do not touch any doors or other hospital equipment during transport.
- On arrival to the ICU, repeat same disconnection procedure (stop ventilation, clamp ETT, disconnect from Ambu / Laerdal bag and connect to ICU ventilator; declamp ETT and start ventilation.
INFECTION CONTROL & DEBRIEF
- Remove PPE per local hospital protocol before leaving the OR / ICU. Doffing is preferably done in an anteroom if available.
- Doffing with utmost care; use buddy system.
- If doffing is done in the OR, do this at the corner of the room and at least > 6 feet away from patient (droplet zone).
- Remember to remove the N95 mask last once you have left the OR.
- Some protocols suggest taking a shower after a contaminated COVID case.
- All surfaces of equipment and supply must be wiped down when the drape is removed.
- All contaminated equipment e.g., the suction device, ETT, nasogastric tube (if used) and even the tape to cover the eyes must be handled carefully and discarded.
- Team debriefing
- Staff to complete personal log book of clinical exposures
ADDITIONAL RESOURCES
Guidelines for Surgical Patients with COVID +ve Result
Scheduled: Scheduled surgical patients must be tested for COVID-19 by nasopharyngeal swab within 72 hours before planned surgery. For patients who have tested COVID +ve, refer to Guidelines for Surgical Patients with COVID+ Result. Outpatients must be advised to self-isolate at home until their surgery. In addition, all patients arriving to the surgical admission unit will undergo syndromic surveillance to identify the presence of fever, upper respiratory tract infection symptoms and new gastrointestinal symptoms.
Algorithm for Managing COVID-19 Surgical Patients
Tracheal intubation for critical ill adults with COVID-19
Click HERE for addional resources